Device Closure Procedure for ASD and PDA at Rhythm Heart & Critical Care Hospital, Nagpur by Dr. Manish Juneja
Dr. Manish Juneja, a leading cardiologist at Rhythm Heart & Critical Care Hospital in Nagpur, specializes in advanced cardiac treatments, including the Device Closure Procedure for Atrial Septal Defect (ASD) and Patent Ductus Arteriosus (PDA). These congenital heart defects can significantly impact heart function, and the Device Closure Procedure offers a minimally invasive solution to correct these issues.
What is ASD and PDA?
- Atrial Septal Defect (ASD): ASD is a hole in the wall (septum) that separates the two upper chambers of the heart (atria). This defect allows oxygen-rich blood to mix with oxygen-poor blood, causing the heart and lungs to work harder.
- Patent Ductus Arteriosus (PDA): PDA is a persistent opening between the aorta and the pulmonary artery, which normally closes after birth. If left untreated, PDA can lead to heart failure or other complications.
What is a Device Closure Procedure?
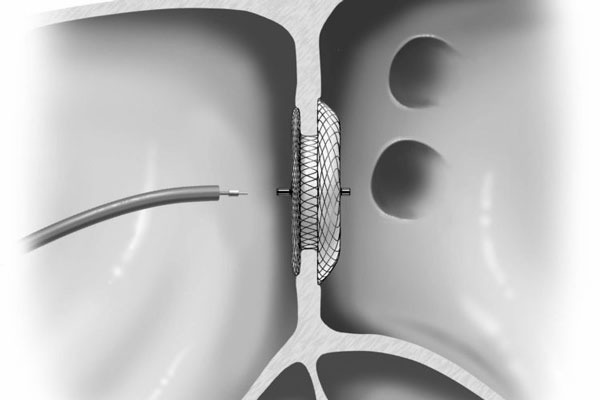
The Device Closure Procedure is a minimally invasive technique used to close the abnormal openings in the heart caused by ASD or PDA. It involves the insertion of a specialized device through a catheter, which is guided to the site of the defect to seal it effectively.
Why is a Cardiac Closure Device Used?
A cardiac closure device is used to prevent the complications associated with ASD and PDA, such as heart failure, stroke, and arrhythmias. This device helps restore normal blood flow, reducing the strain on the heart and improving overall cardiac function.
How is the Procedure Performed?
The procedure is performed using a catheter that is inserted into a blood vessel in the groin. The catheter is carefully guided to the heart, where the closure device is deployed to cover the defect. The device then expands and securely seals the opening, allowing the heart to function normally. The procedure is typically completed under general anesthesia and requires only a short hospital stay.
What are the Advantages of an ASD Closure Device?
- Minimally invasive with a quicker recovery time compared to open-heart surgery.
- Reduced risk of complications and scarring.
- Immediate improvement in symptoms and heart function.
- Lower chance of long-term complications related to ASD or PDA.
Types of Closure Devices Used
There are different types of closure devices used in this procedure, tailored to the specific needs of the patient:
- Amplatzer Septal Occluder: Commonly used for ASD closure, this device is designed to securely close the defect and integrate with the heart tissue over time.
- Nit-Occlud Device: Often used for PDA closure, this device is made of a flexible, nitinol wire mesh that conforms to the shape of the defect and ensures a secure closure.
Post-Procedure Care and Recovery
After the Device Closure Procedure, patients typically stay in the hospital for observation for 24 to 48 hours. During this time, doctors monitor the patient’s heart function and ensure the device is properly positioned. Patients can usually return to normal activities within a week, although strenuous activities should be avoided for several weeks. Regular follow-up appointments are crucial to monitor the success of the procedure and the patient’s recovery.
Potential Risks and Complications
While the Device Closure Procedure is minimally invasive and generally safe, there are potential risks and complications, including:
- Device displacement or migration.
- Blood clots forming around the device.
- Infection at the catheter insertion site.
- Arrhythmias (irregular heartbeats) following the procedure.
Long-Term Outcomes of Device Closure
The long-term outcomes of the Device Closure Procedure are highly favorable, with most patients experiencing significant improvements in heart function and quality of life. The closure devices are designed to last a lifetime, reducing the need for further interventions. Regular monitoring through echocardiograms and other tests ensures that the device remains effective and that the heart continues to function optimally.
Innovations in Device Closure Technology
Advancements in medical technology have led to the development of more effective and safer closure devices. Newer devices are smaller, more flexible, and easier to deploy, making the procedure even less invasive and improving patient outcomes. Dr. Manish Juneja’s practice is at the forefront of adopting these innovations, ensuring that patients receive the most advanced care available.
Why Early Intervention Matters
Early diagnosis and intervention for ASD and PDA are crucial in preventing long-term complications. Delaying treatment can lead to irreversible damage to the heart and lungs. The Device Closure Procedure offers a timely solution that not only addresses the defect but also prevents further deterioration of the patient’s health.
What Makes the Device Closure Procedure Minimally Invasive?
The Device Closure Procedure is considered minimally invasive because it is performed using a catheter-based approach rather than traditional surgery. This means:
- No Large Incisions: Only a small incision is made in the groin area to insert the catheter, reducing the risk of infection and scarring.
- Less Pain: Patients experience less post-procedure pain and discomfort compared to open-heart surgery.
- Faster Recovery: With a shorter hospital stay and quicker return to daily activities, patients benefit from a faster overall recovery.
Cost-Effectiveness of the Device Closure Procedure
The Device Closure Procedure is also a cost-effective alternative to open-heart surgery. With fewer complications, shorter hospital stays, and quicker recovery times, the overall cost of treatment is often lower. This makes it a financially viable option for many patients and healthcare systems.
Continued Monitoring and Follow-Up Care
Long-term follow-up care is essential for patients who have undergone the Device Closure Procedure. Regular check-ups, including echocardiograms, are scheduled to monitor the heart’s function and ensure that the closure device remains effective. Dr. Manish Juneja and his team provide comprehensive follow-up care, addressing any concerns and adjusting treatment as needed to ensure optimal long-term outcomes.